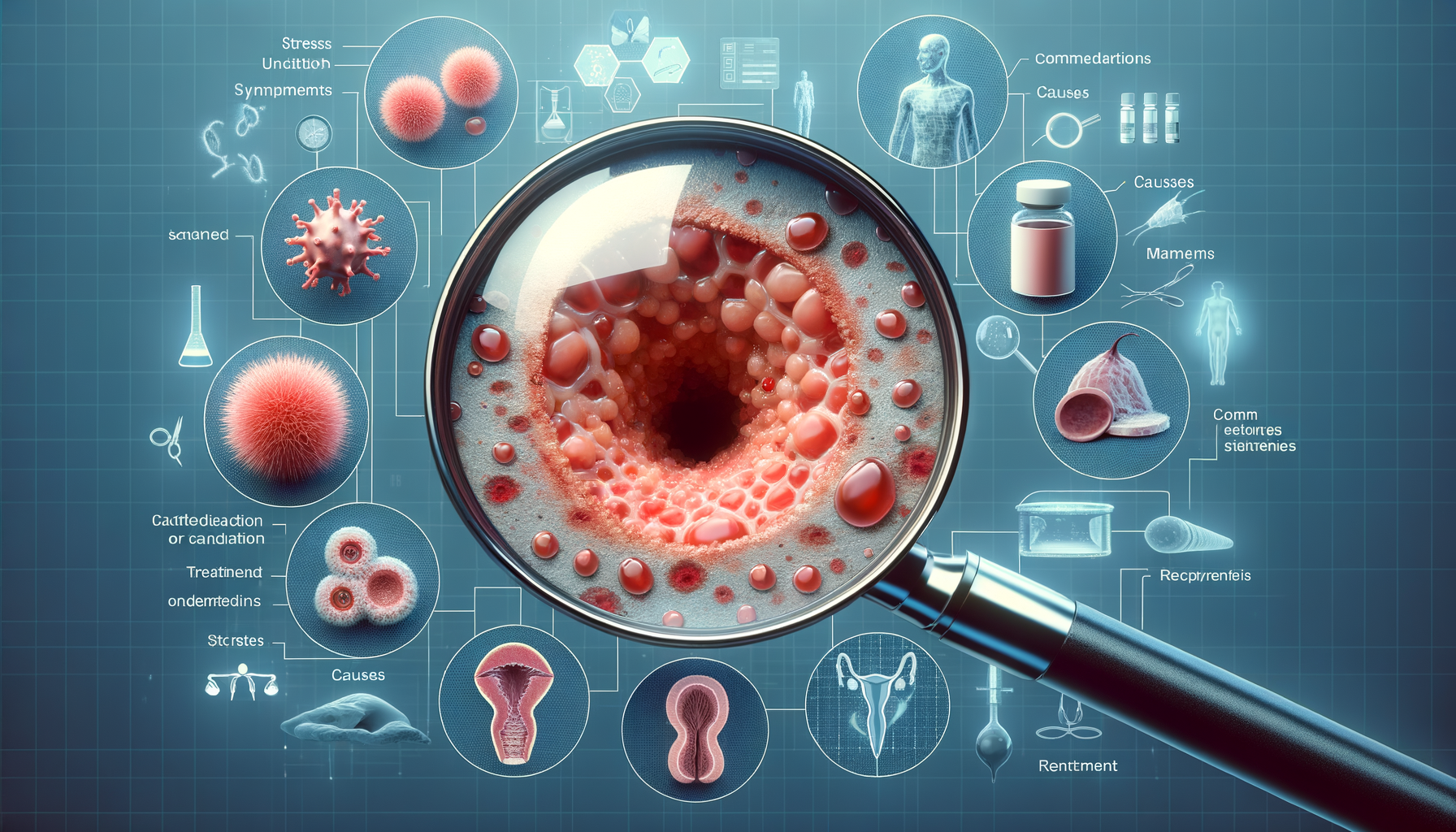
Introduction to Genital Psoriasis
Psoriasis is a chronic skin condition that affects millions worldwide, characterized by red, scaly patches on the skin. While it can manifest on various parts of the body, genital psoriasis is a particularly sensitive form of the condition. This type of psoriasis can have a significant impact on an individual’s quality of life, affecting both physical comfort and emotional well-being. Understanding genital psoriasis is crucial for those affected, as it can guide them toward effective management strategies and improve their overall quality of life.
Genital psoriasis requires careful attention due to the delicate nature of the skin in this area. Unlike psoriasis on other parts of the body, genital psoriasis often lacks the thick scales typically associated with the condition, making it more challenging to diagnose. This article delves into the common symptoms, potential causes, and triggers of genital psoriasis, providing a comprehensive overview to enhance awareness and understanding.
Common Symptoms and Signs
Genital psoriasis can present in various ways, and its symptoms may differ from psoriasis on other parts of the body. The most common signs include red, inflamed patches of skin that may appear smooth and shiny. These patches can occur on the pubic area, upper thighs, and the skin folds around the genitals. Unlike typical psoriasis, genital psoriasis often lacks the thick, silvery scales, which can make it less recognizable.
Other symptoms may include:
- Itching or burning sensation in the affected area
- Discomfort during sexual intercourse
- Sensitivity or pain due to friction
The symptoms can vary in intensity, with some individuals experiencing mild irritation while others may face significant discomfort. It’s important to note that genital psoriasis can coexist with other forms of psoriasis, such as plaque psoriasis, which might be present on other parts of the body.
Due to its location, genital psoriasis can also have psychological effects, including embarrassment and anxiety, which further underscores the need for proper diagnosis and management.
Causes and Triggers
The exact cause of psoriasis, including genital psoriasis, remains unknown. However, it is widely believed to be an autoimmune condition, where the immune system mistakenly attacks healthy skin cells, leading to rapid skin cell growth and the formation of psoriatic lesions. Genetic factors also play a significant role, as psoriasis tends to run in families.
Several triggers can exacerbate genital psoriasis, including:
- Stress: Emotional stress is a well-known trigger for psoriasis flare-ups.
- Infections: Certain infections, such as streptococcal throat infections, can trigger or worsen psoriasis.
- Skin injuries: Cuts, scrapes, or friction in the genital area can provoke a psoriasis outbreak.
- Medications: Some medications, including lithium and beta-blockers, can trigger or worsen psoriasis.
Understanding these triggers is crucial for managing genital psoriasis effectively. Individuals with psoriasis should work closely with healthcare providers to identify personal triggers and develop strategies to minimize flare-ups.
Management and Treatment Options
Managing genital psoriasis requires a tailored approach, considering the sensitive nature of the affected area. Treatment options typically include topical treatments, which are applied directly to the skin. These may include corticosteroids, vitamin D analogs, and calcineurin inhibitors, which help reduce inflammation and control symptoms.
In addition to medications, lifestyle changes can significantly impact the management of genital psoriasis. These changes may include:
- Maintaining a healthy weight to reduce skin friction
- Wearing loose-fitting, breathable clothing to minimize irritation
- Practicing stress-reduction techniques such as meditation or yoga
For individuals with severe symptoms, systemic treatments such as biologics or phototherapy may be recommended. It’s important for individuals to work closely with their healthcare provider to determine the most appropriate treatment plan based on the severity of their condition and their overall health.
Regular follow-ups with a dermatologist can help monitor the condition and adjust treatments as necessary, ensuring optimal management of genital psoriasis.
Conclusion: Living with Genital Psoriasis
Living with genital psoriasis can be challenging, but understanding the condition and its triggers can empower individuals to manage their symptoms effectively. By recognizing the common signs and symptoms, identifying personal triggers, and exploring treatment options, those affected can take proactive steps to improve their quality of life.
Education and awareness are key components in managing genital psoriasis. By staying informed and working closely with healthcare professionals, individuals can navigate the complexities of this condition with confidence and resilience. While there is currently no cure for psoriasis, effective management strategies can significantly reduce symptoms and enhance overall well-being.
Ultimately, a comprehensive approach that includes medical treatment, lifestyle adjustments, and emotional support can make a significant difference for those living with genital psoriasis.


Leave a Reply