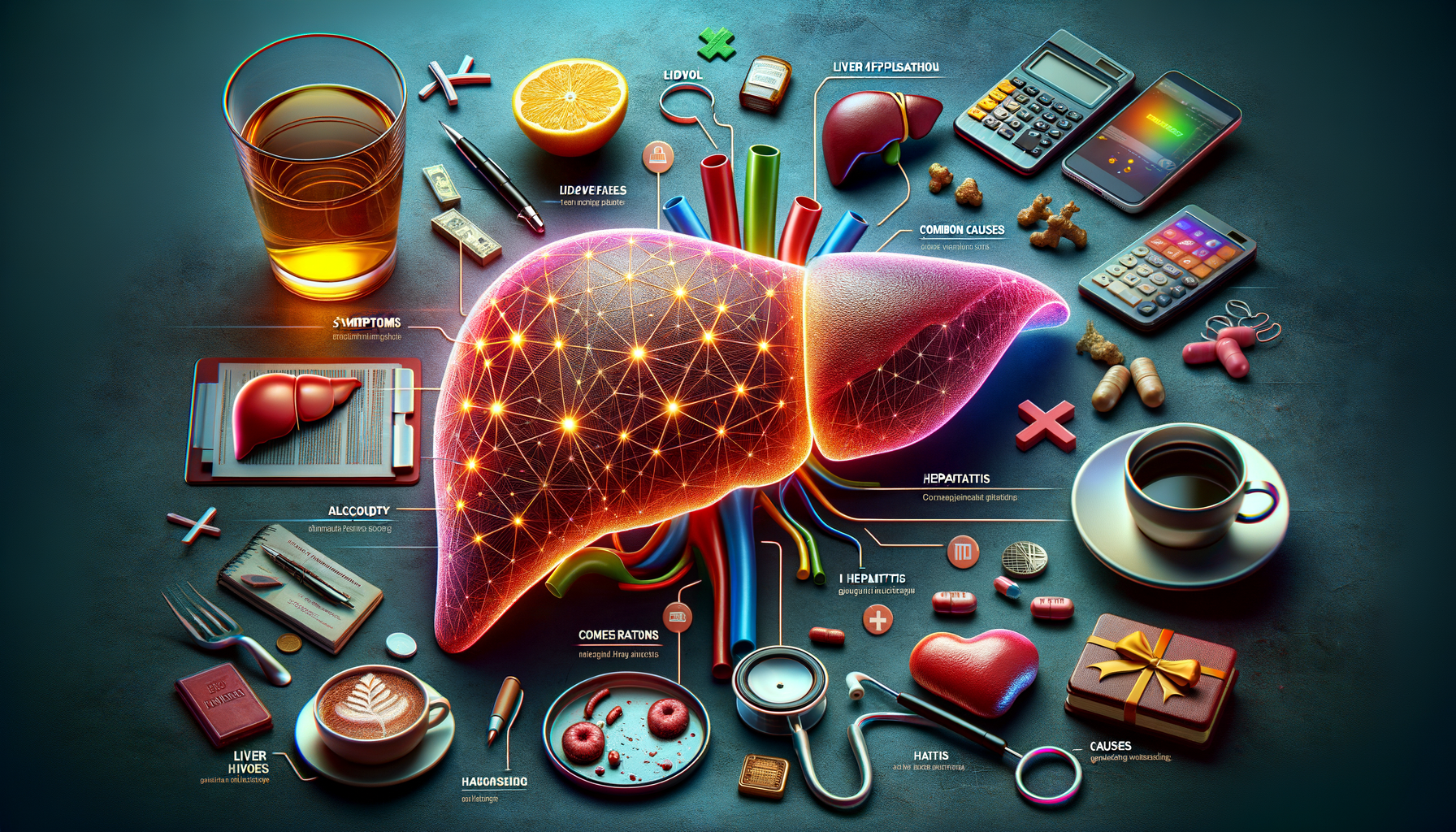
Understanding the Symptoms of Liver Cirrhosis
Liver cirrhosis is a condition that gradually deteriorates liver function. Recognizing the symptoms early can be the key to managing the condition effectively. Here are five symptoms that may indicate liver cirrhosis:
- Fatigue: As the liver’s efficiency declines, the body experiences increased fatigue, making even simple tasks exhausting.
- Jaundice: This is characterized by a yellowing of the skin and eyes, resulting from the liver’s inability to process bilirubin effectively.
- Swelling: Fluid retention in the abdomen (ascites) and legs (edema) is a common symptom due to impaired liver function.
- Bruising and Bleeding: A cirrhotic liver produces fewer proteins necessary for blood clotting, leading to easy bruising and bleeding.
- Confusion: Known as hepatic encephalopathy, this occurs when toxins build up in the brain due to the liver’s reduced detoxification ability.
Identifying these symptoms early can prompt individuals to seek medical advice, potentially slowing the progression of the disease.
How Cirrhosis Affects Overall Liver Function
The liver is a vital organ responsible for numerous critical functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion. Cirrhosis severely impacts these functions, leading to a cascade of health issues.
One of the primary roles of the liver is detoxifying the blood. In cirrhosis, scar tissue replaces healthy liver tissue, obstructing blood flow and leading to toxin accumulation. This can result in hepatic encephalopathy, where toxins affect brain function, causing confusion and cognitive impairments.
Protein synthesis is another crucial function. The liver produces proteins essential for blood clotting. With cirrhosis, the production of these proteins diminishes, increasing the risk of bleeding and bruising. Additionally, the liver’s role in regulating cholesterol and glucose levels is compromised, potentially leading to metabolic disorders.
Furthermore, cirrhosis affects bile production, necessary for fat digestion and absorption. This can result in malnutrition and deficiencies in fat-soluble vitamins, further exacerbating health issues. The cumulative effect of these dysfunctions underscores the liver’s central role in maintaining overall health and the severe implications when its function is compromised.
Common Causes and Risk Factors for Cirrhosis
Cirrhosis can result from various causes, often linked to lifestyle choices and underlying health conditions. Understanding these can help in taking preventive measures.
One of the most prevalent causes is chronic alcohol abuse. Excessive alcohol intake over time damages liver cells, leading to inflammation and scarring. Another significant cause is chronic hepatitis infections, particularly hepatitis B and C, which cause long-term liver inflammation and damage.
Non-alcoholic fatty liver disease (NAFLD) is also a growing cause of cirrhosis, often associated with obesity, diabetes, and metabolic syndrome. This condition leads to fat accumulation in liver cells, causing inflammation and scarring over time.
Other risk factors include:
- Genetic Disorders: Conditions such as hemochromatosis and Wilson’s disease can lead to cirrhosis due to abnormal accumulation of iron and copper, respectively.
- Bile Duct Disorders: Diseases like primary biliary cholangitis can cause bile duct damage, leading to cirrhosis.
- Autoimmune Diseases: Autoimmune hepatitis involves the body’s immune system attacking liver cells, causing inflammation and scarring.
Recognizing these causes and risk factors is crucial for early intervention and lifestyle modifications to prevent the progression of cirrhosis.
Managing Liver Cirrhosis: Treatment and Lifestyle Adjustments
While cirrhosis is a serious condition, management strategies and lifestyle adjustments can significantly improve quality of life and slow disease progression. Treatment typically focuses on addressing the underlying cause and alleviating symptoms.
For alcohol-related cirrhosis, abstinence from alcohol is crucial. Support groups and counseling can be beneficial in maintaining sobriety. In cases related to hepatitis infections, antiviral medications can help control the virus and reduce liver damage.
Dietary changes are also essential. A balanced diet rich in fruits, vegetables, and lean protein supports liver health. Limiting salt intake can help manage fluid retention, while avoiding raw or undercooked shellfish reduces the risk of infections.
Regular monitoring by healthcare professionals is important to track liver function and manage complications. In advanced cases, liver transplantation may be considered as a treatment option, offering a potential cure for cirrhosis.
Overall, a proactive approach involving medical treatment, lifestyle changes, and regular monitoring can help manage cirrhosis effectively, improving outcomes for those affected by this condition.
Conclusion: Taking Charge of Liver Health
Liver cirrhosis is a progressive disease with significant health implications. By understanding its symptoms, effects on liver function, and common causes, individuals can take proactive steps toward prevention and management. Early detection and lifestyle modifications play a crucial role in managing cirrhosis and maintaining overall health.
Awareness and education about liver health are vital. Regular medical check-ups, healthy lifestyle choices, and avoiding risk factors can help protect this essential organ. By taking charge of liver health, individuals can improve their quality of life and reduce the risk of serious complications associated with cirrhosis.


Leave a Reply