Prostate Cancer
Understanding Prostate Cancer
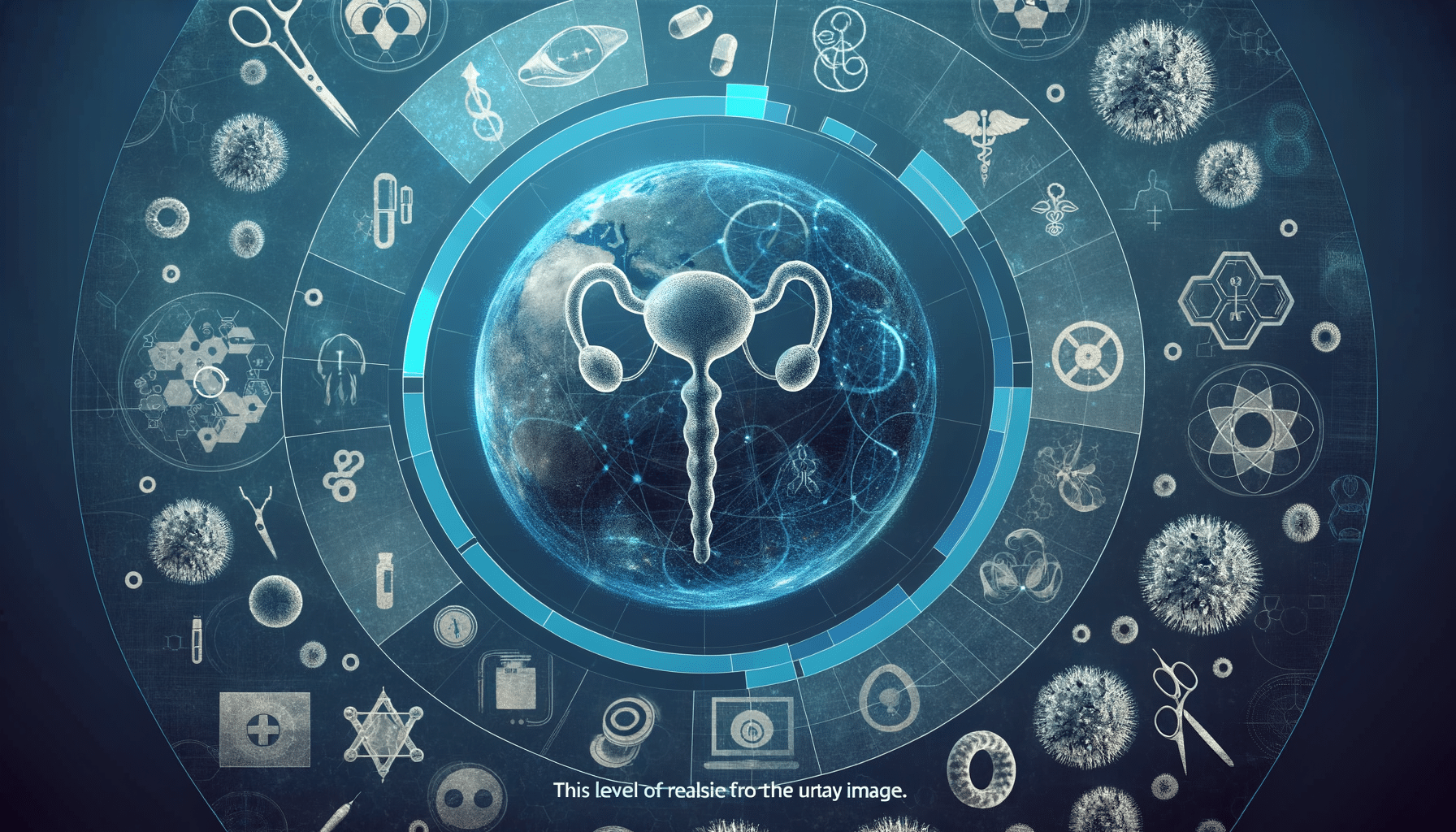
Prostate cancer is a significant health concern, particularly for men over the age of 50. It is a cancer that occurs in the prostate, a small walnut-shaped gland in men that produces seminal fluid. This type of cancer is among the most common in men, and understanding its nature and progression is crucial for effective management. The prostate gland is located below the bladder and in front of the rectum, and its primary function is to produce fluid that nourishes and transports sperm.
One of the challenges with prostate cancer is that it often develops slowly and may not show symptoms until it is in an advanced stage. This makes regular screening and early detection vital. The risk of developing prostate cancer increases with age, and it is more prevalent in certain ethnic groups, with African American men having a higher incidence rate.
Prostate cancer is generally classified into two types: aggressive and non-aggressive. Non-aggressive prostate cancer grows slowly and may not require immediate treatment, while aggressive types can spread quickly and need prompt intervention. Understanding these differences can help in making informed decisions about treatment options.
Symptoms and Diagnosis of Prostate Cancer
Prostate cancer symptoms can vary and may not be apparent in the early stages. However, as the cancer progresses, symptoms may include difficulty urinating, decreased force in the stream of urine, blood in the urine or semen, and pelvic discomfort. It’s important to note that these symptoms can also be caused by other conditions, such as benign prostatic hyperplasia, which is a non-cancerous enlargement of the prostate.
Diagnosis of prostate cancer typically involves a combination of tests. The prostate-specific antigen (PSA) test is a blood test that measures the level of PSA in the blood, with higher levels suggesting the possibility of prostate cancer. Digital rectal exams (DRE) are also used to detect abnormalities in the texture, shape, or size of the prostate gland. If these tests indicate potential cancer, a biopsy may be performed to confirm the diagnosis.
Early detection through regular screening is crucial, especially for those with a family history of prostate cancer or other risk factors. Discussing screening options with a healthcare provider can help in determining the appropriate timing and frequency of tests.
Risk Factors and Prevention
Various risk factors can influence the likelihood of developing prostate cancer. Age is the most significant risk factor, with the majority of cases occurring in men over 50. Family history is another important factor; men with a father or brother who had prostate cancer are at increased risk. Additionally, certain genetic mutations, such as those in the BRCA1 and BRCA2 genes, have been linked to a higher risk of prostate cancer.
Diet and lifestyle also play a role in prostate cancer risk. A diet high in red meat and high-fat dairy products and low in fruits and vegetables may increase the risk. Conversely, maintaining a healthy diet rich in vegetables, fruits, and whole grains can help reduce the risk. Regular physical activity and maintaining a healthy weight are also beneficial in lowering the risk of prostate cancer.
While some risk factors, such as age and genetics, cannot be changed, adopting a healthy lifestyle can help reduce the risk of prostate cancer. Regular check-ups and discussions with healthcare providers about personal risk factors and screening options are essential components of prevention.
Treatment Options for Prostate Cancer
Treatment for prostate cancer depends on several factors, including the stage of the cancer, the patient’s age, overall health, and personal preferences. Common treatment options include active surveillance, surgery, radiation therapy, hormone therapy, and chemotherapy.
Active surveillance may be recommended for non-aggressive prostate cancer, where the cancer is monitored closely without immediate treatment. This approach is suitable for older men or those with other health issues where the risks of treatment may outweigh the benefits.
Surgery, such as a prostatectomy, involves the removal of the prostate gland and is often used for cancer that is confined to the prostate. Radiation therapy uses high-energy rays to target and kill cancer cells and can be administered externally or internally.
Hormone therapy aims to reduce the levels of male hormones that can fuel the growth of prostate cancer cells. Chemotherapy may be used for advanced prostate cancer that has spread beyond the prostate gland.
Each treatment option has potential side effects and long-term implications, so it is crucial to discuss these with healthcare providers to make an informed decision that aligns with personal health goals and lifestyle.
Coping and Support for Prostate Cancer Patients
A prostate cancer diagnosis can be overwhelming, not only for the patient but also for their family and loved ones. It is essential to have a strong support system and access to resources that can help navigate the emotional and physical challenges of the disease.
Support groups and counseling services can provide a platform for sharing experiences, advice, and encouragement. Many organizations offer resources specifically for prostate cancer patients, including educational materials, support networks, and financial assistance programs.
Maintaining open communication with healthcare providers is crucial for managing treatment side effects and adjusting care plans as needed. Patients should feel empowered to ask questions and advocate for their health needs throughout the treatment process.
In addition to medical support, lifestyle changes such as a balanced diet, regular exercise, and stress management techniques can improve overall well-being and quality of life for prostate cancer patients. Engaging in activities that bring joy and fulfillment can also be a valuable part of the healing process.