Genital Psoriasis
Understanding Genital Psoriasis
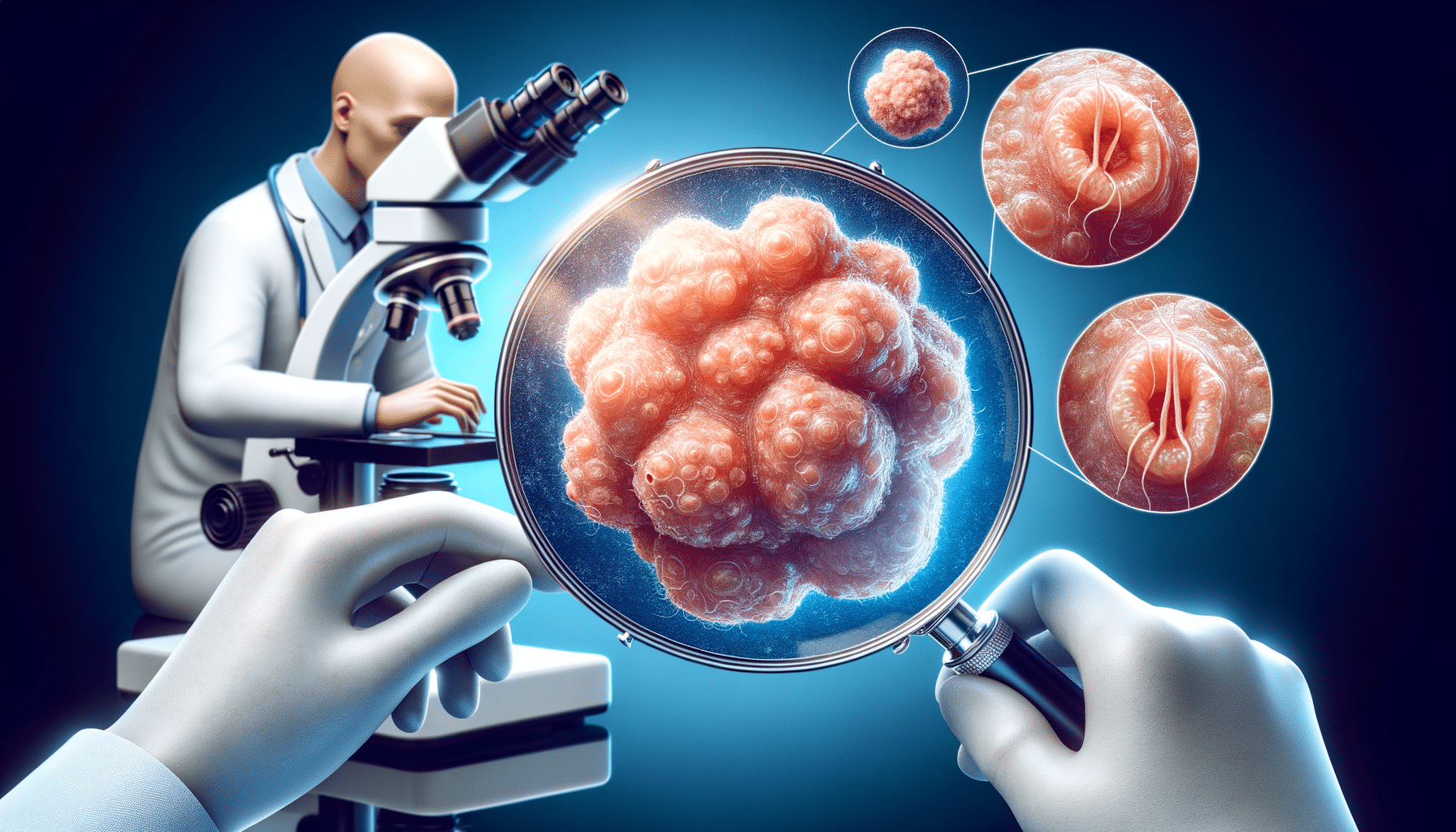
Psoriasis is a chronic autoimmune condition that affects the skin, leading to the rapid growth of skin cells and the formation of scales and red patches. When psoriasis affects the genital area, it poses unique challenges due to the sensitivity and the need for careful management. Genital psoriasis can manifest in various forms, such as small red patches, dry skin, or even lesions that can cause significant discomfort.
The skin in the genital region is thinner and more sensitive compared to other parts of the body, which means that the symptoms of psoriasis can be more pronounced and uncomfortable. This sensitivity requires special attention when diagnosing and treating the condition. While genital psoriasis is not contagious, the stigma and embarrassment associated with it can affect a person’s self-esteem and intimate relationships.
Common symptoms of genital psoriasis include itching, pain, and redness. These symptoms can often be mistaken for other skin conditions, making accurate diagnosis by a healthcare professional crucial. Understanding the specific presentation of psoriasis in this sensitive area is essential for effective treatment and management.
Diagnosis and Challenges
Diagnosing genital psoriasis can be challenging due to its similarity to other conditions such as eczema, fungal infections, or sexually transmitted infections. A thorough examination by a dermatologist is often necessary to differentiate between these conditions. In some cases, a biopsy may be required to confirm the diagnosis.
The challenges of diagnosing genital psoriasis are compounded by the emotional impact it can have on individuals. Feelings of embarrassment or discomfort discussing symptoms with healthcare professionals can lead to delays in diagnosis and treatment. It is important for individuals to overcome these barriers and seek professional help to ensure proper care.
Once diagnosed, the treatment of genital psoriasis needs to be tailored to the individual’s specific needs. The delicate nature of the skin in this area requires gentle treatment options that minimize irritation while effectively managing symptoms. This often involves a combination of topical treatments and lifestyle adjustments.
Treatment Options
Treating genital psoriasis requires a careful balance between efficacy and gentleness. Topical treatments are commonly used, including low-potency corticosteroids, which help reduce inflammation and itching. However, prolonged use of corticosteroids can lead to skin thinning, so they must be used under medical supervision.
Other topical treatments include calcineurin inhibitors, which are effective in reducing inflammation without the side effects associated with steroids. These treatments are particularly suitable for sensitive areas such as the genitals. In some cases, phototherapy may be recommended, although its application in the genital area is limited due to the risk of skin damage.
Beyond medical treatments, lifestyle changes can play a significant role in managing genital psoriasis. Maintaining good hygiene, wearing loose-fitting clothing, and avoiding irritants such as harsh soaps or detergents can help reduce symptoms. Additionally, stress management techniques and a healthy diet can support overall skin health.
Psychological and Emotional Impact
The psychological and emotional impact of genital psoriasis can be profound. The condition can affect a person’s self-image and confidence, particularly in intimate situations. The fear of judgment or rejection can lead to anxiety and depression, further exacerbating the condition.
Support from healthcare professionals, family, and support groups can be invaluable in helping individuals cope with the emotional challenges of genital psoriasis. Open communication with partners about the condition can also help alleviate fears and strengthen relationships.
Therapy or counseling may be beneficial for those struggling with the psychological effects of the condition. Addressing these emotional aspects is an important part of a comprehensive treatment plan for genital psoriasis.
Living with Genital Psoriasis
Living with genital psoriasis requires a proactive approach to management and self-care. Regular follow-ups with a dermatologist can help monitor the condition and adjust treatment plans as needed. Staying informed about new treatments and research developments can empower individuals to make informed decisions about their care.
Building a support network of healthcare professionals, friends, and family can provide the necessary emotional and practical support. Sharing experiences with others who have the condition can also offer comfort and reduce feelings of isolation.
Ultimately, while genital psoriasis presents unique challenges, it is a manageable condition with the right approach. By prioritizing gentle care, seeking professional advice, and addressing emotional well-being, individuals can lead fulfilling lives despite the condition.